I teach improvisational theatre to health scientists and trainee doctors. When I tell people this, they are often confused because theatre and medicine appear to be separate fields.
Medicine, however, is a performance. And the skills actors and improvisers learn are equally important for any health-care role.
A theatre professor once told me theatre skills are life skills. When I trained as an actor, I needed to learn how to communicate my ideas clearly. I was trained to collaborate and actively listen, to be present and react quickly in the moment.
Theatre also allowed for an experience in which I could step into the life of a character and see the world from their perspective.
For more than 10 years now, I have been facilitating theatre courses within undergraduate health science and medical education—to enhance the clinical skills of students and train better health-care professionals.
A medical improv curriculum
If you think about it, the doctor- or surgeon-patient encounter is like improv, requiring two characters, in role, to build a scene together.
Improvisers must think creatively and adapt in the moment. In the same way, health professionals must learn to respond creatively and with mental agility in rapidly changing circumstances, under time pressure, sometimes in life-and-death situations—while maintaining their professional composure.

Improvisational theatre can also offer a way for health-care professionals to combat burnout and compassion fatigue.
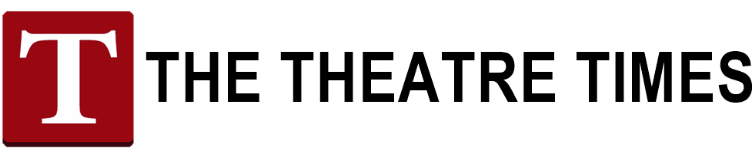
(Shutterstock)
Currently, I am facilitating a medical improv curriculum with the Department of Family and Community Medicine at Sunnybrook Health Sciences in Toronto.
Medical improv is defined as “the adaptation of improvisational theatre principles and training techniques to improve communication, cognition, and teamwork in the field of medicine.” The goal is to enhance clinical skills and build knowledge related to the seven roles of a competent physician defined by Canada’s Royal College of Physicians and Surgeons.
I have also taught theatre and improv in the Bachelor of Health Sciences (Honours) program at McMaster University since 2007. While this is not a health professional program, many students end up pursuing careers in healthcare.
It is equally important to expose these students to theatre before they enter health professional programs as it allows for deeper reflection, awareness, and skill development at an earlier stage.
Acting cuts through stereotypes
Fundamentally, acting is about empathy. Actors must understand what a character wants in a scene. When students are assigned a role, some can be initially critical of characters because they have negatively stereotyped them based on their own lived experiences and personal biases.
Through theatre, participants are able to embody the other. Through this process, health-care professionals may deepen their understanding, learn something new about the experience of an illness and develop greater empathy for their patients.
If you were to watch doctors in a theatre session, on the surface they might be waddling around like penguins or twirling like spaghetti. But they are learning how to communicate, how to support patients, and how to collaborate together. It’s play but it’s serious play.
Reflective discussion after exercises is essential, allowing for learning, discovery, and growth. The participants are able to make meaning of their own experience. The method is fun, but the content is serious.
Free to fail, without consequence
Serious play can be incredibly valuable—not only to enhance skills but also address burnout and compassion fatigue, which is becoming an increasing problem in Canadian medical schools.
Within the theatre space, medical students are free to explore and experiment without restrictions. They can try out ideas, make mistakes and fail without consequence.
The work is not about teaching doctors and health professionals to fake empathy; it is about using theatre as a way to enhance creativity and clinical skills.
As researchers Gretchen Case and Daniel Brauner argue, it allows “doctors to identify and critique the professional roles that they play daily and to choose their words and gestures deliberately so that their interactions with patients become more empathetic, compassionate, and thoughtful.”![]()
This article originally appeared in The Conversation on September 16, 2018, and has been reposted with permission.
This post was written by the author in their personal capacity.The opinions expressed in this article are the author’s own and do not reflect the view of The Theatre Times, their staff or collaborators.
This post was written by Hartley Jafine.
The views expressed here belong to the author and do not necessarily reflect our views and opinions.